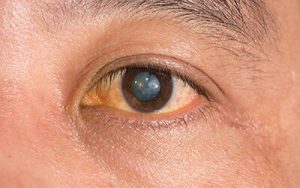
Infections
Eye infections are seen frequently and some of the causes are due to cosmetics and/or makeup brushes. Makeup brushes are recommended to be cleaned frequently as it collects dirt, dust or bacteria overtime. If left uncleaned, an infection may develop. Also, if a product is expired or not properly concealed, it can be contaminated. Symptoms one may notice includes irritation, redness, teary, and discharge. It is important to discontinue makeup that causes these symptoms and use proper hygiene.
Allergic reactions
Not every makeup product is made for everyone as it may cause an allergic reaction. Be sure to check the label and ingredients before purchasing a new product, especially a product that you have not used before. Reactions can cause swelling to the eyes, puffiness, itchiness, redness and irritation to the eye.
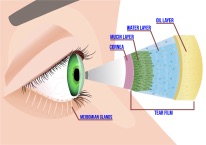
Scratched cornea
While applying eye makeup, accidents can happen causing a scratch or damage on the cornea, the front of the eye. This causes an abrasion which can be very uncomfortable. Symptoms to be aware of include pain, light sensitivity, difficulty opening the eye, decreased vision, tearing and redness. If not treated, it can potentially cause a serious infection to the eye.
Safety tips to keep eyes safe
● Wash your hands before applying eye cosmetics to avoid infections.
● Make sure that any cosmetics you place near the eye is clean.
● Do not use old containers for eye cosmetics.
● Do not share your cosmetics, especially eye makeup brushes. Another person’s bacteria in your cosmetics can be harmful to you.
● Do not use eye cosmetics if you have an eye infection or the skin around the eye is red.
● Introduce one new makeup product at a time. If an allergic reaction occurs and multiple new products were used, it can be difficult to determine which caused the reaction.
● When applying or removing makeup, be careful and remove with care.
● Avoid expired products.
● Remove makeup products thoroughly before bedtime.
If you are experiencing symptoms and believe it may be due to makeup use, contact your eye doctor to avoid further complications.
Author: Dr. Ia Ong Her
July 26, 2021